I talked to our benefits department and they found an 85-page plan detail document from 2017 that clearly states if I qualified for Medicare because of ESRD, our insurance plan would be primary and Medicare would be secondary. This is contrary to the last claim details I received. Our benefits coordinator requested a callback from a supervisor from our insurance and he verified that our plan should be primary. He also said he would ask his team to reprocess my claims again to make sure they were paid out correctly. Yay! I was afraid I had to mediate between insurance plans if both thought they were secondary insurance.
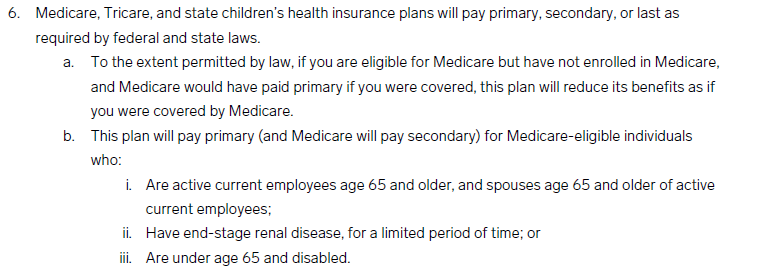
Like my sister, our benefits coordinator said this coordination of benefits when you have multiple insurance coverage is the most complicated topic in health insurance. No one wants to be the primary coverage insurance since they usually paid 80%-85% of the claim. I avoided getting Medicare because of this coordination mess, and only got it because my work insurance will stop paying for dialysis soon.
2 thoughts on “Coordination of Benefits, Part II”