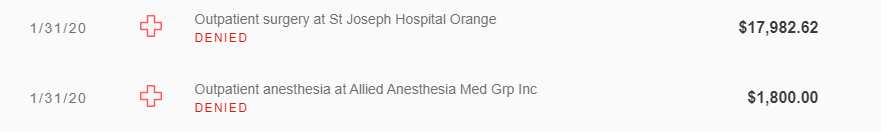
I’m so frustrated with all this. I called our work insurance service provider again today and spoke to the claim supervisor. It turned out he has been out sick so he never got back to me. Anyway, their conclusion is that after 30-months of dialysis, Medicare becomes the primary insurance for all claims. Therefore, I need to have all my providers bill Medicare first, then any remaining amount will be paid by my work insurance. The problem is that Medicare starts three months after the first dialysis date of July 5, 2017, so by rejecting claims after January 5, 2020, my insurance is off by three months. The rules are so confusing that each time I call my insurance or Medicare, the answer seems to change. I’m now getting invoices for this failure of benefits coordination.
Because of this confusion, I’ve stopped seeing my therapist and acupuncturist. I also have several upcoming appointments to see the cardiologist, primary care physician, endocrinologist, and others. I feel like I need to postpone those appointments until the insurance situation is cleared up. My work insurance also started rejecting my cardiac rehab claims so I’m not sure how to continue there since the hospital doesn’t seem to want to bill Medicare on my behalf.