Just got a 10 minute lesson on fluid removal from the head dialysis nurse. There is an attachment on the machine that measures fluid volume in the blood plasma. I think the gist is that fluid is always being transported from cells to tissue space to bloodstream. However, if you can’t make urine, then the fluid stays in your bloodstream, which causes high blood pressure and excess fluid can backup in your organs (e.g, lungs).
This supports my theory that I’ve been losing tissue mass but retaining fluids. By keeping my “dry” weight somewhat constant, I’m actually retaining too much fluid. This was pretty evident a few months ago when I had difficultly breathing and a CAT scan showed ~500 mL of fluid in my lungs. It’s better now since they lowered my weight but it’s probably not enough. My lower leg and ankles are still swollen sometimes and my breathing is not back to 100% yet.
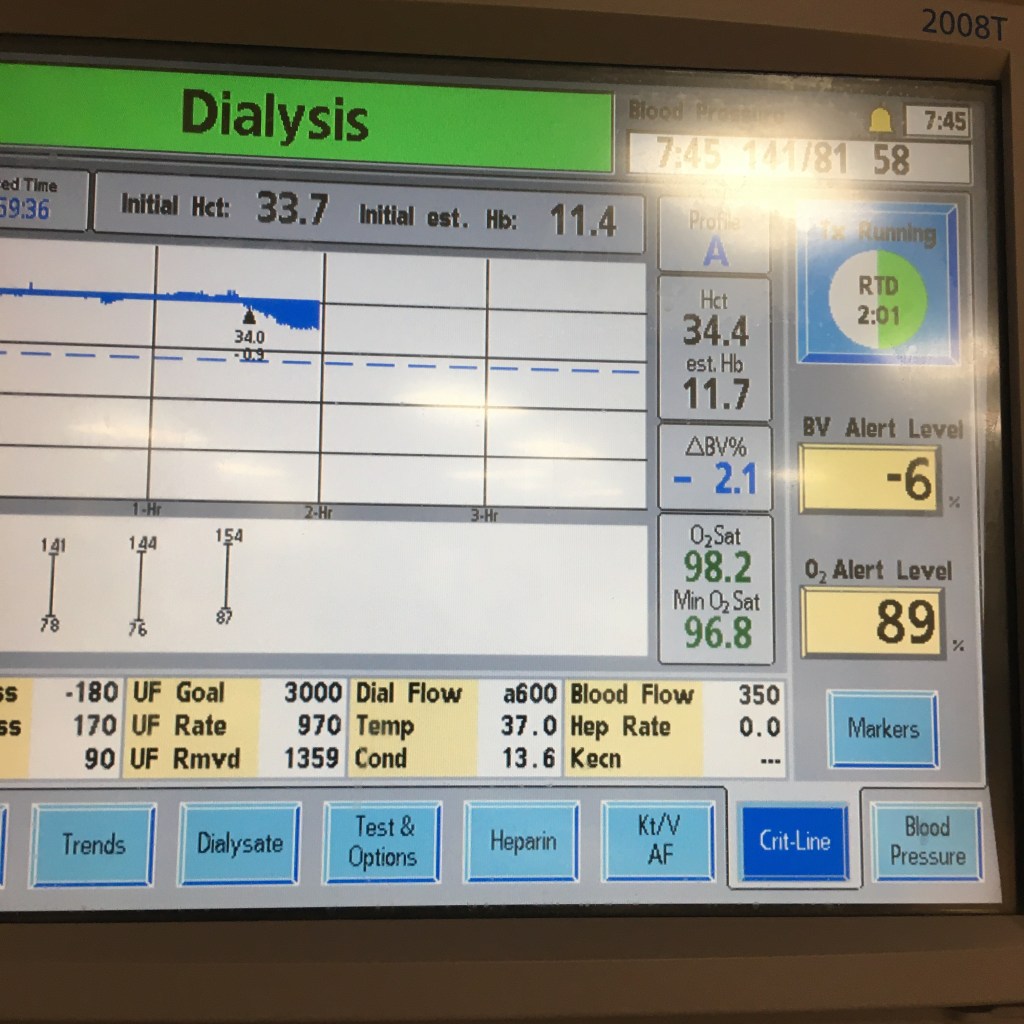
The above is a new screen on the machine that I haven’t seen before. It shows the change in fluid volume in post-dialysis blood. Before the marker on the graph, the change was around zero, which means my body was transporting the same amount of fluid to my bloodstream as the machine was removing. It’s basically saying we need to increase the rate of fluid removal to effectively reduce blood volume. I think the previous rate was 640 mL/ hour, and now it’s up to 970 mL/ hour. You can see the difference in the chart after the marker. My blood pressure is also dropping, which is normal for dialysis. I think the last systolic reading was 157 over something. Previously, since the blood volume was pretty constant and my medication for high blood pressure was being dialyzed out, my blood pressure was actually increasing. This also means that my weight post-dialysis will probably drop some more.
I did ask the nurse why they don’t run this analysis on every patient every session. She said most patients are stubborn and have lots of opinions about their treatment, especially how much fluid to remove. That seems crazy to me; why would I know more about dialysis than the nephrologist/nurse/technician? This device takes the guesswork out of determining the right amount of fluid removal. They’re going to do this a few more sessions to pinpoint the optimal fluid removal rate.
Science!
==========
We had to turn off the ultrafiltration part of dialysis about 30 minutes from the end since I was feeling dizzy, and my systolic blood pressure dropped to 103. I didn’t get a photo of the Crit-Line screen but the blue area was decreasing at the end, and my blood pressure starting increasing a bit. I think the systolic number got to 128 at the end of the session and I no longer felt dizzy. I left the dialysis center at 79.0 kg, which is the lowest weight recorded so far. We’re going to use the device again on Saturday since the nurse thinks there is more excess fluid to remove, but we’re going to start on a higher ultrafiltration rate and lower it over time, instead of starting low and going high at the end. This should reduce the risk of hypovolemic shock.