Initially, I ended the previous post with a paragraph regarding an article on ProPublica written by the same journalist that contacted me nine months ago. However, as I read the first few paragraphs of the story, I felt it needed its own post for discussion.
ProPublica is a nonprofit newsroom that investigates abuses of power.
ProPublica begins all their stories with the above line. It pretty much tells the reader their biases and how they will tell the story. After reading the first few paragraphs, I was not wrong.
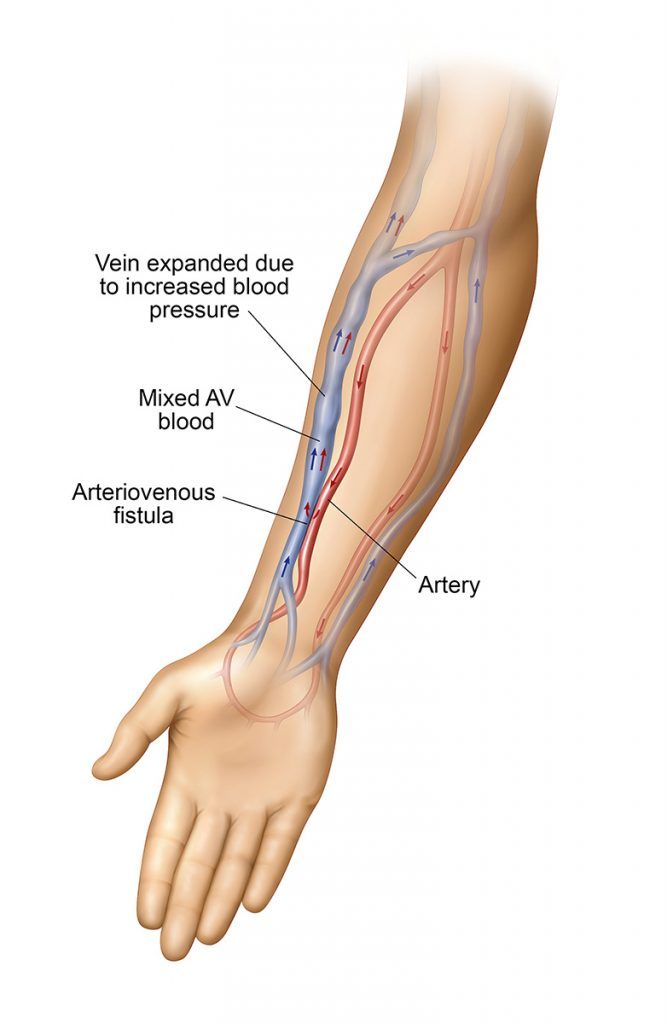
First, there are plenty of things that are wrong with the dialysis industry. I came up with the following just from memory (no Google):
- Two for-profit companies control 70% of the market
- Medicare coverage provides distorted incentive to maintain the status quo and milk the system for profit
- Very little public awareness on the impact of dialysis on ESRD patients
- Even less awareness on the need for organ donation
Just from the recent ballot proposition fights in California between the for-profit dialysis companies and SEIU (employee union) demonstrates even the industry cares only about profits and not patients.
Having said that, ProPublica is obviously biased against dialysis and transplant providers. First, if I assume my interview request in September 2020 is related to this story, the timing is a bit off. The actual article was published on December 15, 2020, but the subject of the article passed away earlier in August. So, by the time I was contacted, they already had most of the information needed for the article. What did they need my story for? A supplemental article about how getting a transplant suck for everyone?
If you read about the life of JaMarcus Crews, it is definitely a more compelling story than if they had written about me. JaMarcus was was black, living in Alabama, and likely experienced a lot of discrimination/racism in life and the whole dialysis/transplant process. Me, being a middle class Asian in California and getting relatively good care, will be a boring subject for the story ProPublica wanted to tell.
I found a few questionable items at the very beginning of the article.
When it was over, and all anyone wanted was sleep, JaMarcus drove to the wide parking lot at Target to wait for his cashier’s shift. He missed working at the bank, but a nine-to-five was no longer possible.
It is true that in-center hemodialysis takes up a lot of time, but many people work full-time. ProPublica just says this without any sources or statistics. I worked full-time for the first two years of hemodialysis and during peritoneal dialysis. If JaMarcus was a teller, then he must be at the bank in person, which makes it difficult, but not impossible. He could be assigned different tasks during dialysis days. It heavily depends on how willing employers are to accommodate the employee’s dialysis schedule. I was lucky but also essential to my company, so they were very accommodating.
JaMarcus didn’t tell his wife or son that he was making calculations in his head: most people didn’t survive five years on dialysis. He was nearing seven. His mother had died in year eight.
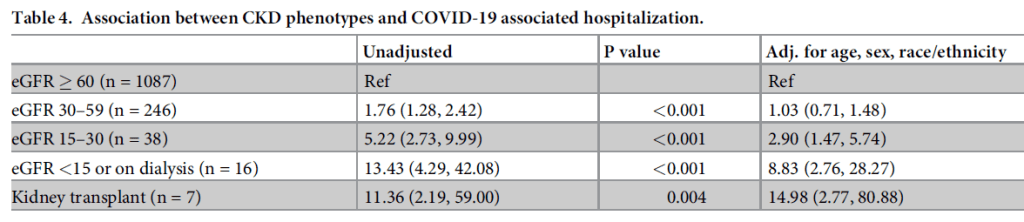
This one is totally false and can be researched with a quick Google search. I posted on this topic a lot, and most sources say that mortality is 20% after the first year of dialysis, and 50% after five years. That is definitely not “most people didn’t survive five years on dialysis.” The statistics are also skewed by older dialysis patients with multiple medical issues. JaMarcus was 36. That does not mean there is no risk, since JaMarcus did pass away, but the statement is absolutely false.
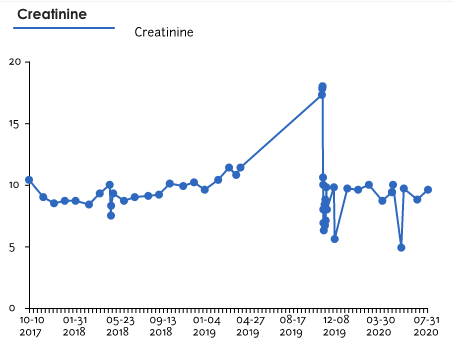
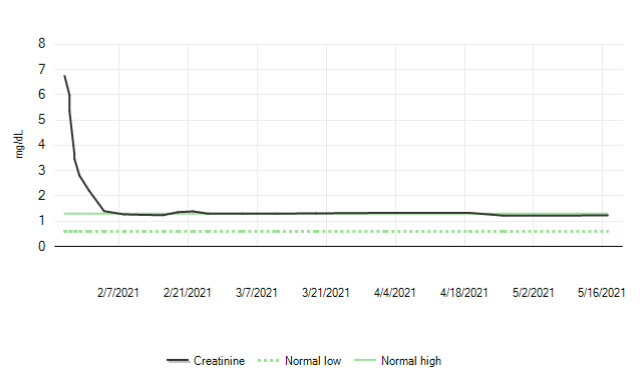
Having gone through all of this, ESRD and dialysis is definitely a huge problem that needs more attention and research. JaMarcus’s story is sad, and not even unique. I know my comments may be premature based on the first few paragraphs, but one-sided stories like these just entrench people and hinder progress. I am still amazed that I am not dead after years of ESRD and dialysis. If you browse through r/transplant on Reddit, there are lots of anniversary stories from transplant recipients. Of course, the process could be better, but I am hugely grateful and satisfied with my experience. Everyone I have engaged with, from my nephrologist, dialysis nurses and techs, transplant coordinators, surgeons, post-care doctors, to phlebotomists, have been compassionate and caring. The main issue is the scarcity of transplant organs that causes all these issues downstream. ProPublica should focus on that part of our society, but that does not fit their mission of investigating the abuse of power.
Maybe I will change my mind after reading the entire article.
==========
Just saw these lines at the very top of the story:
For years, JaMarcus Crews tried to get a new kidney, but corporate healthcare stood in the way.
He needed dialysis to stay alive. He couldn’t miss a session, not even during a pandemic.
That is lame. Whatever you think about “corporate healthcare” in general, JaMarcus weighed 400 pounds and had heart problems. There is no way he was going to get on any transplant list when healthy people must wait 8-10 years. I can see him getting a transplant if there were lots of organs available, but with only 10% of people on the waitlist transplanted each year, he needs to improve his health situation. No way this is the fault of “corporate healthcare.” Also, WTF is “corporate healthcare?” Of course, it is large hospitals (corporations) doing transplants. You do not want the procedure done in someone’s garage, for fuck sakes.
I also do not understand the second sentence. I had to go to my clinic during COVID pandemic. That is the only place I went outside of my house. Even without a pandemic, dialysis patients cannot miss sessions since that will mess up your health even worse. Is this the fault of “corporate healthcare” too? How is this racism? I thought ProPublica was like NPR: a good news source that leans a bit left. But so far, this seems like a total hit piece.
In hindsight, I am glad the journalist did not follow-up. I would be really pissed off if I were part of this story the way it was told.