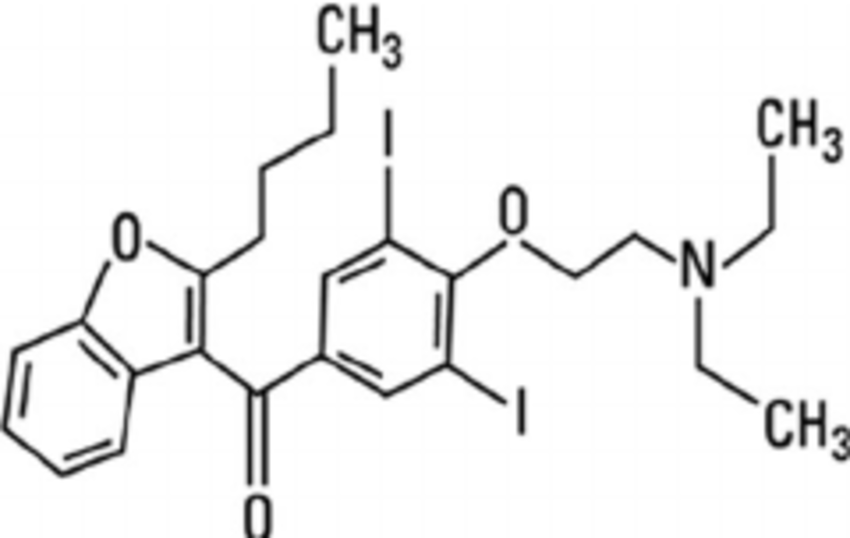
Back when my a-fib started, my regular cardiologist prescribed me to take 400 mg of Multac twice a day. It’s an anti-arrhythmia medication similar to amiodarone (I guess they all have the -darone ending) but with less side effects. Here’ some more info from their website.
What are possible serious side effects from taking MULTAQ?
MULTAQ may cause serious side effects including slowed heartbeat, inflammation of the lungs (including scarring and thickening), low potassium and magnesium levels in your blood, and changes in kidney function blood tests.
What are the most common side effects?
The most common side effects when taking MULTAQ include stomach problems such as diarrhea, nausea, vomiting, stomach area pain, and indigestion; feeling tired and weak; skin problems such as redness, rash, and itching. Tell your doctor about any side effect that bothers you or that does not go away.
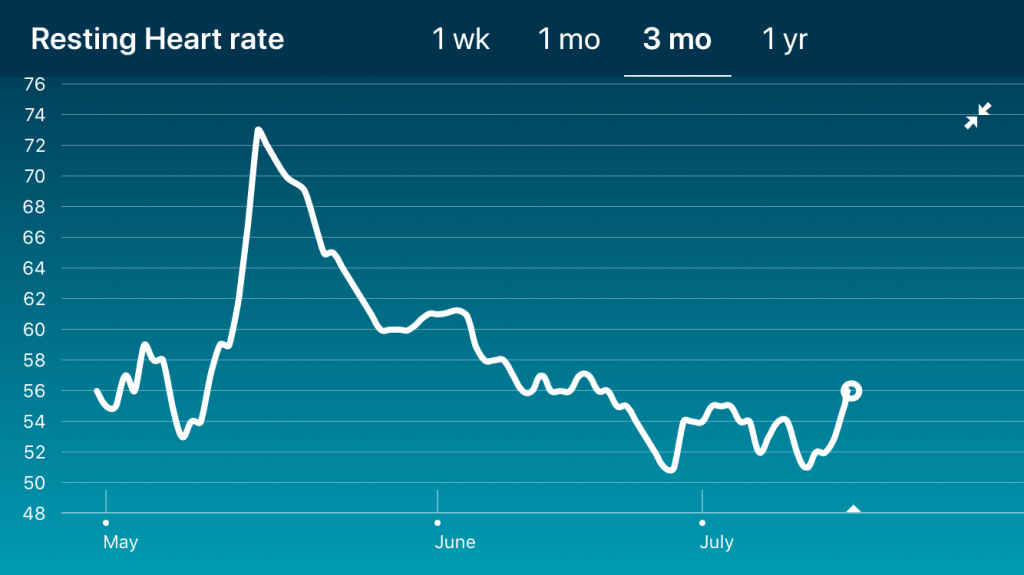
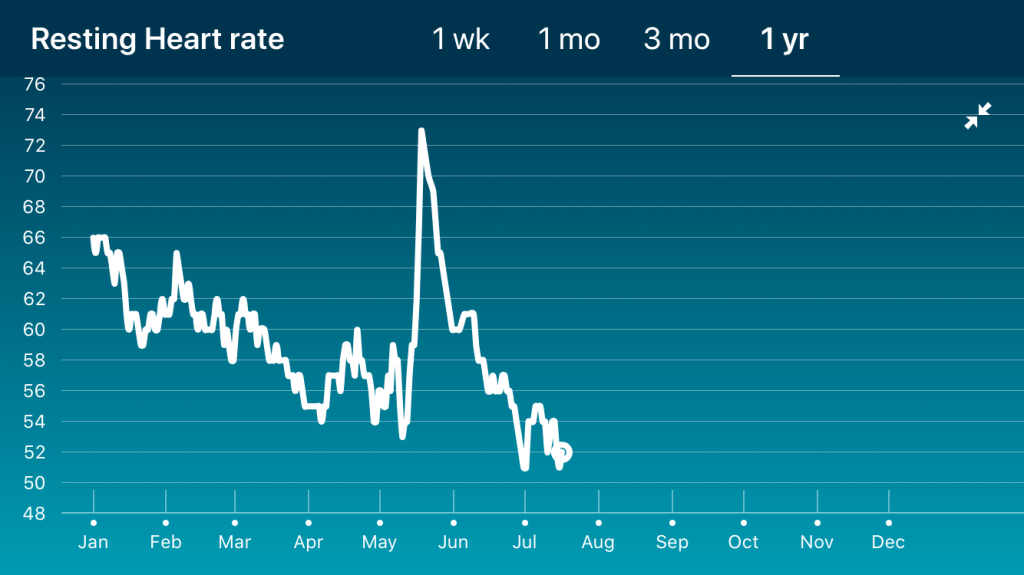
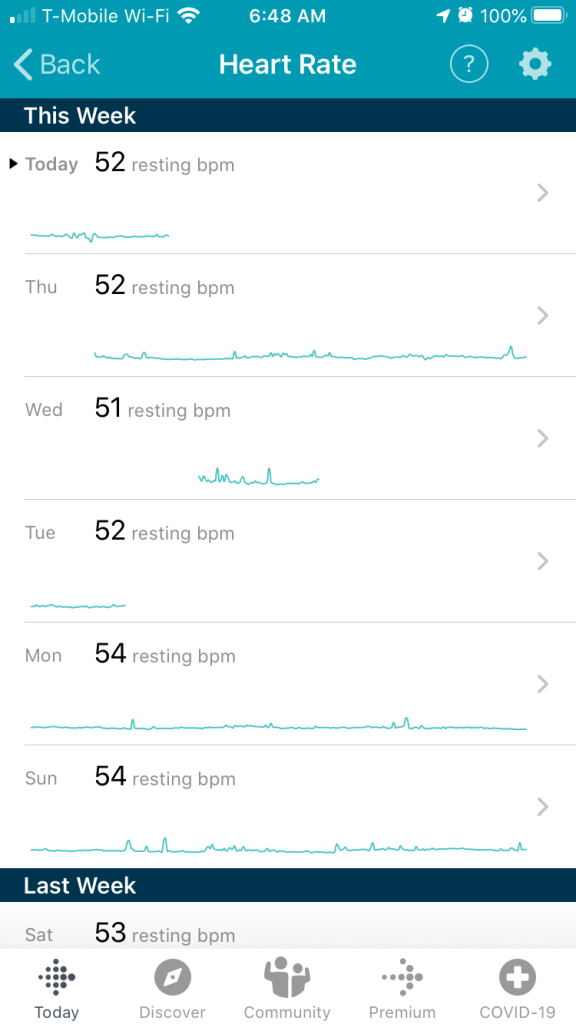
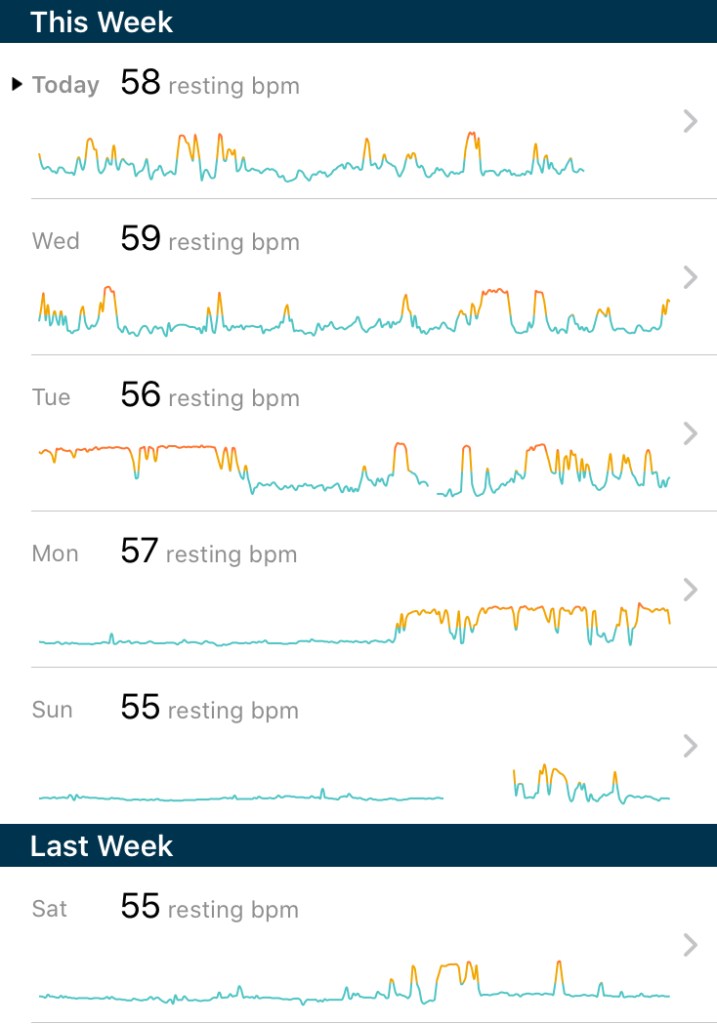
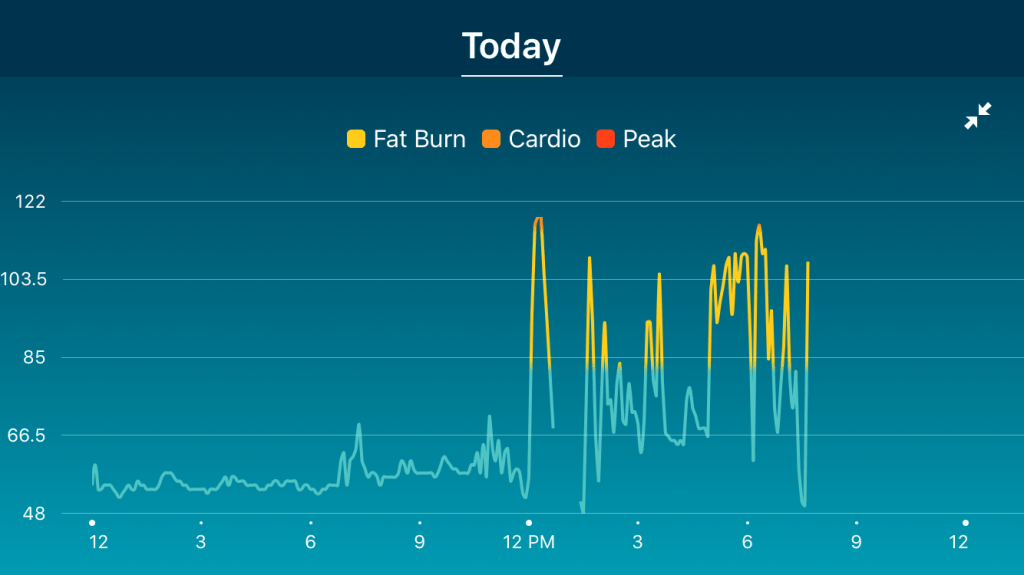
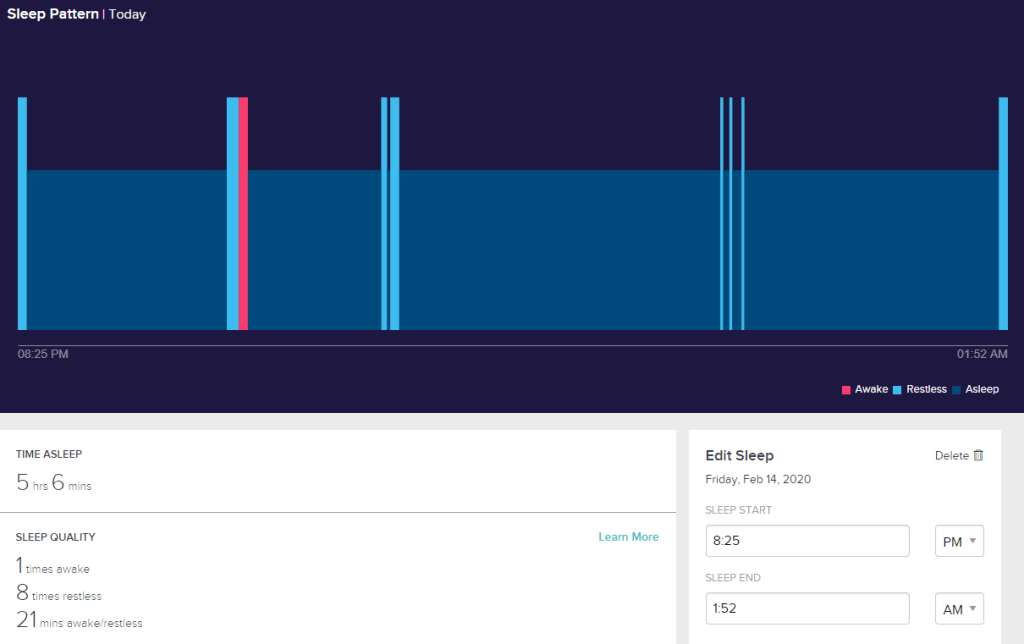
I think I was experiencing some of the side effects while taking Multec. For sure I was vomiting more often. It was mailing at meal times but lots of fool smell or taste would trigger a reflex reaction. I think at one point I was throwing up 4x in one week. I also think my slower than normal heartbeat post-ablation is partially due to the Multac as well. Before a-fib, my heart rate was in the mid- to upper-50’s. With ablation + Multac, I was seeing high 40’s and low 50’s. Now that I’ve stopped taking Multec, heart rate seems to be a bit higher and I’m throwing up a lot less. However, if it’s like amiodarone, the half-life of the drug may be pretty long, which means some of the effects will linger for weeks.