The same tech was able to get both needles into my fistula today as well and we ran the machine at 350 mL/min. He did mention that starting Saturday, another tech will try to insert the needles so hopefully he has good luck as well. They have been using the standard 16 gauge needles that should sustain higher flow rates so I’m going to ask them if we can run at 400 or 450 mL/min and possibly cut down on the dialysis time.
Tag: Hemodialysis
Fistula Update 6/30/2020 (updated)
Woohoo! One of the techs that was the first to try and insert needles into my fistula tried again today. Since everyone thinks my veins are both deep and moves around a lot, all the techs try to push the needle perpendicular to my arm to go deep, then dig around to get the blood to flow. This is weird since you can clearly feel the vein right below the skin layer. Anyway, the tech went shallow and got both needles to flow on the first attempt. One of the needles did hurt for the four hours if I moved my arm slightly but they were able to run the machine at 350 mL/min. Sigh… finally. I’m hoping this trend continues so I don’t have to have another surgery on my arm, and they can take out my chest catheter so I can take showers again.
==========
The arterial “wound” is still bleeding after an entire day. I swapped out two band-aids and it has soaked both of them. I think it’s finally stopped bleeding. I’ve seen “accidents” at the dialysis clinic where blood is squirting out of the arterial needle prick point resulting in a huge puddle of blood on the floor. I hope I don’t get that at home.
Fistula Update 6/23/2020
Sigh… fistula didn’t work again today. It did work well last Saturday however they were able to run at 350 mL/min through two needles. I think the nurse really wants me to talk to the vascular surgeon again but he did say that he wasn’t sure the fistula will work when he operated the first time. I’m just tired of all the surgeries.
I wonder what they would do if I didn’t have a chest catheter.
Fistula Update 6/6/2020
Another day another person trying to stick a needle in my fistula. Today, it was one of the senior nurses; my regular nurse is on vacation today. She ended going up further on my forearm and was able to get a good stick. It did hurt when she tried to push fluid back so we’re using it to draw blood and use the catheter to send back.
Also she didn’t use lidocaine so it hurt a lot when she jabbed me.
Fistula Update 5/12/2020

Two needles in my arm today. Machine flow rate is set at 250 mL/min.
Fistula Working Again
One of the older techs came by to insert the needle in my fistula. He was on vacation for the past two weeks and I heard he’s been at that dialysis center the longest. Anyway, it still took him about 3-4 tries to get the right vein. They still used only one needle at 250 ml/min, but dialed the time back to 3:45. My nephrologist was doing rounds today and she didn’t want to bother with the extra 15 minutes.
You can kind of tell the vein is getting larger in my arm. There is a definite bump in my lower arm where you can feel the blood rushing by all the time. And it’s noisy. If I sleep on my right side and my arm is anywhere near the pillow, I can hear the blood whooshing by.
Fistula: Missed Again
My dialysis clinic tried to stick my arm again today. The tech tried a few times but was able to finally hit the vein. However, it hurt a lot, even with lidocaine. The needle was only in for five minutes but hurting more and more, and the machine was giving low pressure alarms. Finally, the decide to pull the needle since the vein may have collapsed. Right now, both tubes are connected to the chest catheter. The needle insertion point also has sharp pain when I cough. That’s new.

This is my arm yesterday. There are two post-op scars and a bunch of pinpricks. The two higher up in the arm were the original attempts. Then they moved down the arm and you can see at least seven needle scabs.
Even More Dialysis
Rounding today was the nurse practitioner instead of one of the nephrologists. She said my labs were good except for the Kt/V number and hemoglobin levels. She agreed that when they run slower using the single needle in the fistula, I’m not getting enough dialysis. For now, as long as they’re running one needle and slower flow rate, my session will be extended to four hours. Great! Another 15 minutes with a huge needle in my arm.
As for the low hemoglobin, I’m getting two iron shots this and next week. She also asked about COVID-19 symptoms. I told her that the cough was from surgery and things have gotten a bit worse with the inadequate dialysis. Overall she didn’t seem too worried about my coughing and shortness of breath since there was no fever.
Walking 4/19/2020
I walked on the treadmill again tonight for a bit. It was about 20 minutes at ~2 miles per hour, and once again I felt fine afterwards. However, when I tried to take a nap this afternoon, my breathing felt worse than before. I had to sit us several times because I felt like I wasn’t getting enough air.
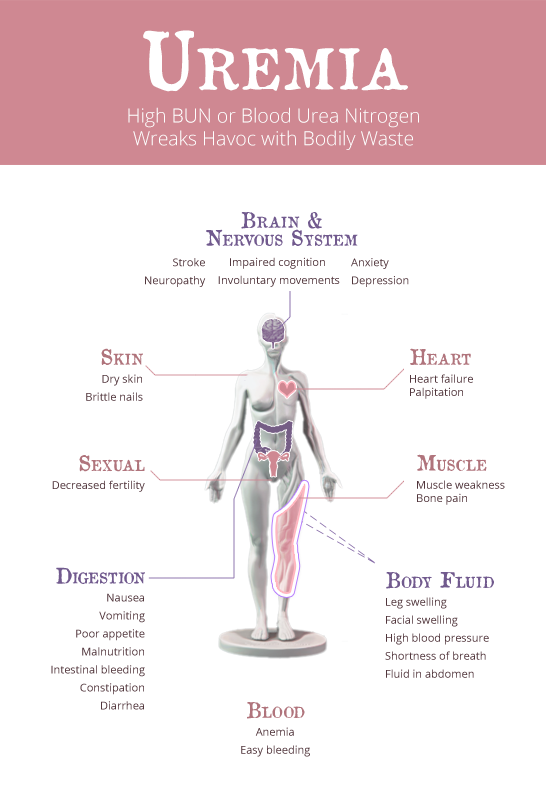
As mentioned before, I think I’m not getting enough dialysis due to the clinic breaking in my fistula. Even running at 250 ml/min, that only gives me ~70% of the dialysis I was getting through the chest catheter at 350 ml/min. I found an article online that lists some symptoms of inadequate dialysis:
- Weight loss (or gain if extracellular volume excess is severe)
- Persistent uremic symptoms, including anorexia, loss of taste, nausea/vomiting, fatigue, pruritus, neuropathy, sleep disturbances, and restless legs.
- Uncontrolled hypertension
- Anemia refractory to treatment
- Uremic pericardial effusion
Fistula: Update 4/18 /2020
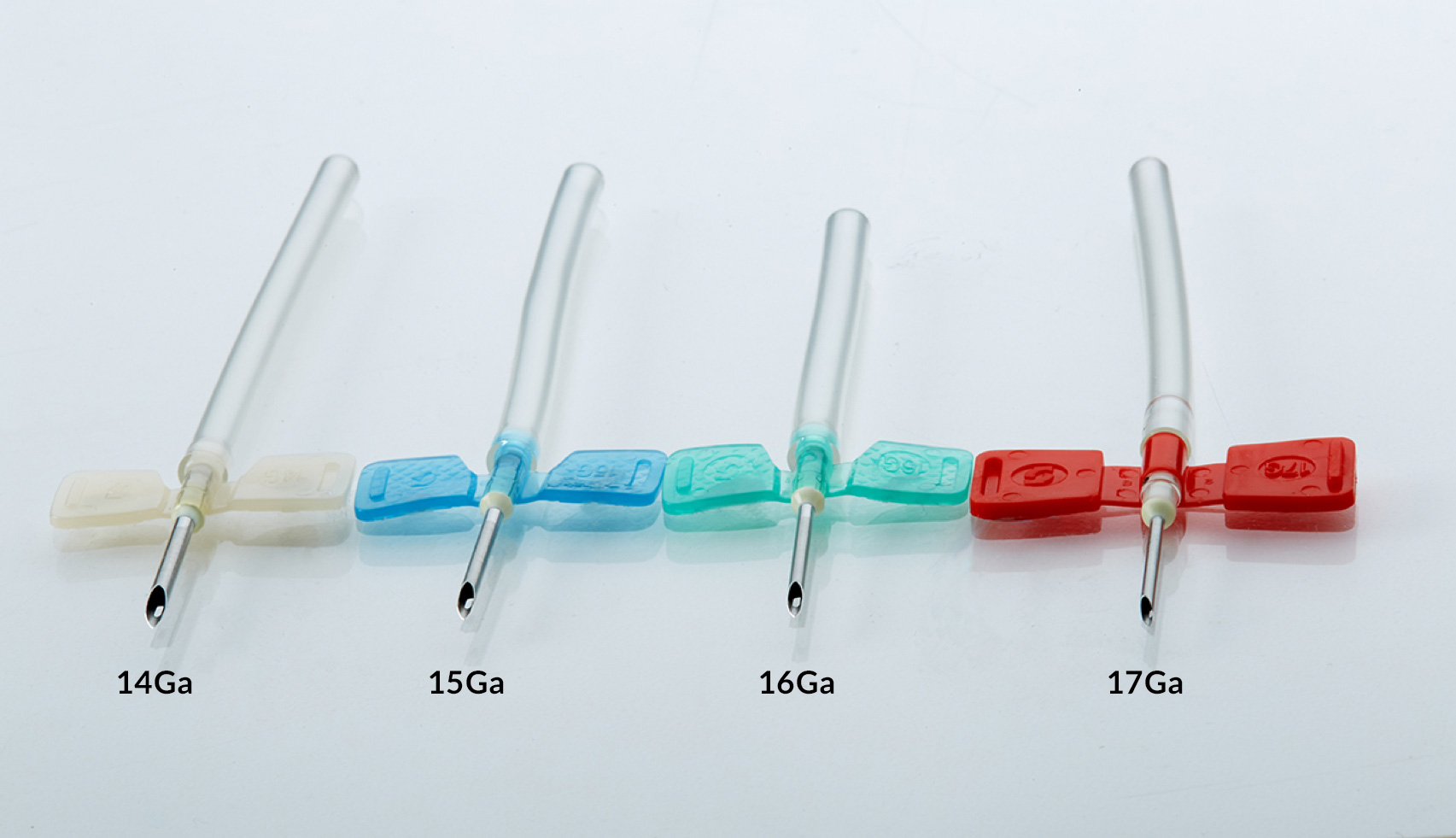
I got called into dialysis early today. Right away the tech tried to stick a needle in my arm. This time she used a regular needle. It was longer and thicker than what they’ve been using on me before. It looked really big and scary. They did give me lidocaine before so it didn’t hurt but now the lidocaine is wearing off, my arm is pretty sore. The machine is running at 250 ml/min so they’re slowly ramping up the flow rate too.
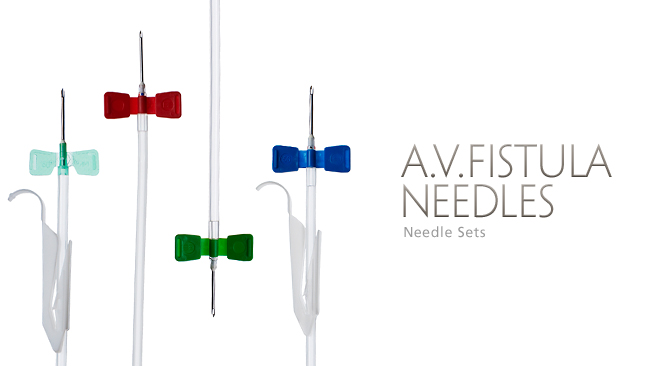
Initially the lead nurse wanted to put two needles in my arm but the tech didn’t think I was ready. Since this was the first time using the regular sized needle (instead of the thinner short needle), we decided to still run one needle in the fistula and use one port in the catheter a few more times.
==========
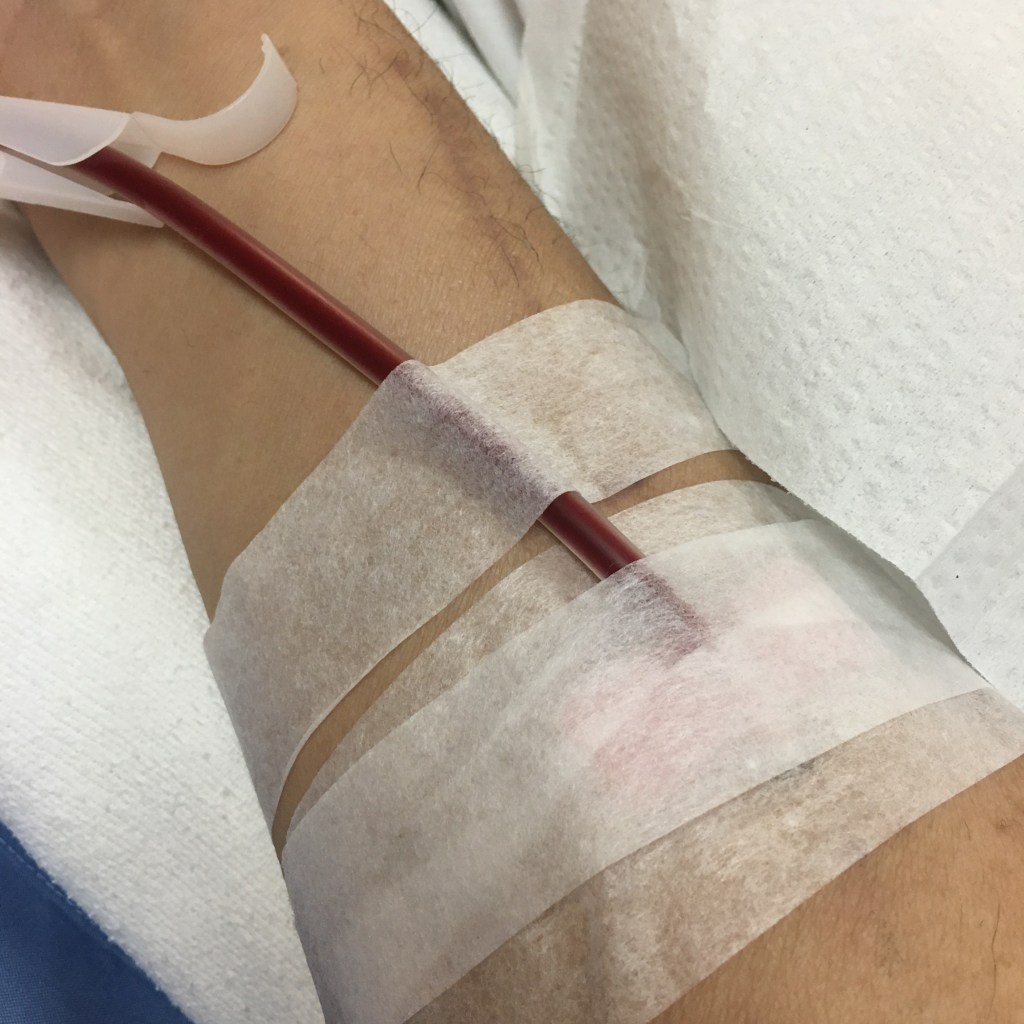
It’s over. It wasn’t too bad during the dialysis session, though I had to actively remember not to move my right arm. It was still sore throughout the entire session but bearable; not sure about having two huge needles though. It did hut a lot more when a different tech pulled the needle out. I only held it for about 10 minutes before she taped me up so I hope it doesn’t bleed everywhere when I take off the tape and gauze.
Fistula: April Labs
I was all ready for them to poke me in the arm again but the dialysis tech said no needles today. I asked them “why” and the reason was April labs. They were drawing blood today for our month labs and one of the tests is dialysis clearance. A blood sample is taken before and after dialysis and the lab determines if the dialysis prescription is adequate. Since they have to run the machine at only 200 ml/min when I’m using the needle, and I barely clear adequacy at 350 ml/min, they didn’t want to use the fistula today since I’ll fail the test for sure. That probably means I’m only getting half dialysis each time they use the needle. I’ve been super tired and running out of breath each time I walk anywhere. Maybe inadequate dialysis is the culprit.
==========
Speaking of labs, the transplant assistant called me yesterday to come in for labs. I told her that I was just there an hour ago (she called at ~1:00 pm) to see the cardiologist. I think she made the appointment for me and then forgot about it. Anyway, I volunteered to drive back to UCLA yesterday but instead, she will ship the test kit to my dialysis clinic to draw samples. They’ve done this several times before and it’s better for me since we can get blood out of my catheter during dialysis without going to a phlebotomist.
Fistula Status 4/14/2020
The tech that inserted the needle in my on Saturday tried the same spot today and was unable to hit the blood vessel cleanly. She tried moving the needle around in my arm several times. Good thing I got lidocane before she started poking. She did get some blood in the needle but when she tried to pull some blood out using a syringe, there was a lot of resistance. She ended up pulling out the needle and we just used the chest catheter today. It did look like she picked up a blood clot in the needle.
About two hours into the dialysis session, one of the supervising nurses came by to try sticking my arm again. My arm was still sore from the first attempt but I told him to go ahead anyway. He was also unable to hit the blood vessel so now I’m 4 for 8 in successful dialysis needle insertions. He said the fistula was pretty good sized so I’m not sure why there’s so many misses. At some point, I will need to remove the chest catheter so they have to insert the needle(s) into the fistula accurately.
Fistula Status 4/11/2020
After today, I’m 4 for 6 on fistula usage. On Thursday, my nurse tried to insert the needle in my arm but did not draw any blood. She is very much a one attempt per needle nurse so she pulled the connector out, put a band-aid on it, and just used the chest catheter for the entire session. Today, a different tech stuck the needle in my arm then made several adjustments with the needle until she was able to hit the blood vessel. Since she did not use any Lidocane, it hurt a lot while she was digging around with the needle. Even afterwards, there was a dull pain at the insertion point for the entire session. Once again, they ran the machine at only 200 ml/min so I’m pretty sure I’m not getting enough dialysis. Is every session going to be like this until the fistula matures more? I can’t imagine sticking two larger gauge needles in at the same time when one thin needle is already hurting.
Fistula: Third Use
The dialysis clinic switched technicians today. They usually rotate the nurses and techs every so often but I can’t figure out their schedule. Anyway, I think my nurse is still out so one of the supervising nurses was substituting. Right at the beginning of the session, one of the techs came over and stuck a needle in my arm. Initially there was no bloodflow but she managed to move the needle a bit and struck the vein. They didn’t use Lidocane this time either so it hurt going in and sporadically during the four hour session. The nurse initially set the flow rate at 200 ml/min but increased it to 220 ml/min. Again, that would mean I was getting less dialysis than necessary since I was barely clearing at 350 ml/min. They did manage to remove 2,600 ml of fluid though.
The nurse asked me to put an ice pack on my arm at home. There was light bruising from the last session. Between surgery scars, Sharpie drawings, needle marks, and bruising, my arm looks like a mess.
Fistula: Intermittent
Since the tech that put the needle in my arm Tuesday is going on vacation, the had another tech try and stick me. She was unable to hit the vein so they’re going to try again later. No lidocaine this time either and it hurt quite a bit. Maybe I need to wait, though everyone at the dialysis clinic wants to use it ASAP.
There’s a older Asian woman next to me getting hooked up and I guess the needles are hurting too. The tech was asking her if she wanted lidocaine. When they stuck me earlier, the tech said the would rather not use lidocaine since it puts an air bubble in the vein and makes subsequent needle insertions harder.
Also, this is the second day in a row where there’s no mask in my supplies bag. I’ve been wearing used surgical masks. Maybe I need to bring my own from now on.
==========
After about an hour and a half, the tech that poked me Tuesday came back and tried again. I think it hurts a lot less if you hit the vein instead of arm tissue. He had to stick the needle almost perpendicularly at first to get at the vein. Anyway, it ended up working and they set the flow rate at 250 ml/min, a small increase from Tuesday. The nurse said they were drawing blood out of my arm and putting it back through my chest. Usually the needle sending cleansed blood back will hurt a lot more if they miss the vein and have blood fill up the tissue around the vein. Great.
Fistula: First Use
About two hours into my dialysis session, one of the techs came by to try out my fistula again. He tried about two weeks ago and got nothing. This time, he was able to hit the vein. However, he didn’t use lidocane this time so I felt every millimeter of the needle going into my arm.

It’s only one needle for now so they disconnected one of the tubes going to my chest catheter and connected it to the fistula tubing. I don’t know which direction the blood is flowing. They also set the flow rate for only 220 ml/min, which is a lot lower than my usual 350 ml/min so I probably didn’t meet my clearance today. There wasn’t a lot of pain; it’s like having an IV needle stuck in you. I hope it doesn’t get worse as they move up in needle size.
After the session ended, the nurse pulled out the needle and put a piece of gauze on the needle site plus a lot of tape. I held the gauze + tape for about 10 minutes then they put more tape over the site and told me not to remove it until 8:00 pm. They also gave me some gauze and tape in case I start bleeding when removing the dressing. Wonderful.
Back From The ER
The patient that got carted out by paramedics Tuesday is back. I didn’t see him on Thurssay someither he came at a different time slot, or had dialysis done in the main hospital. Their room is smaller and much colder.
The patient’s wife is here today watching him. Maybe they made an exception to the no visitors rule since he was just in the ER. He’s sleeping right now but groaning loudly at the same time. Never heard him domthat before and it’s a bit disturbing.
Ugh, my right foot is killing me.
Paramedics at Dialysis Clinic
My dialysis clinic had to call for paramedics again today. Thankfully it was not for me this time. When they called paramedics for me back in December, it ended up with a four hour visit to the emergency room and a whole lot of nothing.
Anyway, there’s a Hispanic man in a wheelchair that had dialysis around the same time as me so I see him in the waiting room, and he’s in the same pod as me. Usually his wife brings him in, but occasionally it’s just a medical transport driver. I’ve never spoken to him in person. I’ve only heard him speak Spanish and he’s usually super grouchy. He’s also confined to the wheelchair so they need to lift him in and out of the dialysis chair.
I’m not sure what was wrong with him today. Usually he’s sleeping in his chair and never seemed to have any issues before. I hope he’s doing okay but the prognosis is not good for dialysis patients with other medical issues.
Transplant Journey
For a long time, I’ve had this nagging feeling in the back of my mind that maybe I’ll never get a transplant and be stuck on permanent dialysis. I look at other people’s transplant experience and it seems so easy. Even at the Kidney Disease Support Group, the leader found out he had kidney failure, sent email out to church group, got 11 offers for donation, and even though he was 74 years old, he received a transplant pretty quickly. Likewise, several other people in the group said they were able to get a transplant shortly after going on dialysis and everything worked out fine.
Then I look back at my journey and it seems like I’m cursed or something. I wrote a long post early on about the last few years of kidney failure. Here’s a summary of transplant expectations that never came to be:
- I was under monthly care of a nephrologist for three years prior do dialysis yet despite all the appointments, tests, and medication, my kidney function kept dropping from eGFR of 50 down to <10.
- Signed up with transplant center at St. Joseph Hospital. Everything was going well until sister was mysteriously rejected by the social worker for non-medical reasons. She believe my sister didn’t really want to donate so she rejected her as a donor.
- We then transferred our transplant wait list time to UCLA with help from a doctor friend. At UCLA, things looked great until the CT scan found a shadow in my sister’s kidney. Not willing to risk cancer, UCLA told us to wait one year. I had to start hemodialysis dialysis while we waited.
- Meanwhile, my high school friend offered to donate. He turned out to be a blood type and 3/6 antigen match. UCLA rejects him due to slightly elevated blood pressure. He then spends the next few years improving his health and eating habits to lose weight and lower his blood pressure. Waiting continues…
- Sister goes back to UCLA after 12 months with new scans showing no sign of cancer. Instead, UCLA asks for a kidney biopsy. During the biopsy procedure, they missed getting a tissue sample. When we asked for a second biopsy, they said no and asked us to wait another 24 months.
- After about 20 months of hemodialysis, the dialysis center and nephrologist really wants me to get a fistula. Instead, I opt for peritoneal dialysis. After surgery and six months of dialysis at home, we determine PD to be a failure and return to hemodialysis. During that time, I was not getting enough dialysis and end up losing my remaining kidney function.
- After persisting for several years, my friend manages to get UCLA’s approval as donor so everyone goes back for more interviews and tests. As we were scheduling the last set of tests, I go to the ER and end up with a quadruple bypass surgery, which puts my transplant on hold.
- After surgery, my friend still wants to donate so UCLA said they would clear me after I complete the cardiac rehab program. I start program in mid-January and is delayed by fistula surgery. Right now, I’m only 14/24 sessions complete.
- When it looks like I’m making good progress and working towards a transplant within months, coronavirus pandemic hits and everything shuts down in the US. I need to call the rehab center to see if they’re still open but with the directive to hospital to focus on respiratory emergencies, I don’t know if UCLA is even working on kidney transplants at this time. Also it doesn’t seem like the right time to start taking immunosupressive drugs required post-transplant surgery.
Along this journey, I kept feeling like a live donor transplant was always imminent. However, each time I take a step forward, some obstacle would appear and block the transplant. I was always worried about either my donor’s health or my health deteriorating before the transplant happened but who would have imagined a global pandemic halting the process? I feel like I have zero control over my future and will be stuck on dialysis the rest of my short miserable life.
Fistula: Not Ready
After hooking me up with the chest catheter, one of the techs tried to stick one needle into my fistula. He gave me some lidocaine first so I didn’t feel anything. He poked a few times and said the fistula wasn’t ready. Usually it takes 2-3 months to mature; my surgery was only ~6 weeks ago. Sometimes it can mature that fast but we’re going to wait a few weeks to try again.
He used the thinnest needle so it wasn’t that scary. Since I’m on the border on clearance, they will probably need to used a larger gauge needle eventually to increase the flow rate. Not looking forward to that unless it can shorten my session time.
Speaking of dialysis, there were a few changes due to COVID-19. Their was a person taking everyone’s temperature at the door, and they’re not letting in visitors in the dialysis clinic. Everyone is wearing a face shield and I’ve gotten my mask so maybe they found more supplies.