I was supposed to start using my new fistula today but I checked out. I told the dialysis nurse to wait until Tuesday instead. While I was in the waiting room, two patients were talking about problems with their fistula. One patient has his completely blocked so he needs surgery. I guess I got freaked out so I’m avoiding it today.
Tag: Hemodialysis
Peripheral Neuropathy 3/11/2020
I think the diphenhydramine in Tylenol PM does have something to do with the increased neuropathy in my feet and legs yesterday. I only slept from 6:00 am to 7:30 am this morning so I’m super tired from basically four days of no sleep. I did go to work while skipping rehab but decided to come home early after a few meetings. I got home around 2:00 pm and slept until 6:00 pm, then again after dinner from 8:30 pm until now-ish. I still need to sleep more but at least I was able to get a few naps in.
The numbness feels like it’s subsided a bit. My feet are still numb but it’s no so unbearable like it was yesterday. I read that the half-life of diphenhydramine is about 6-12 hours so all of it should be gone within 1-2 days. Good thing it’s metabolized by the liver instead of the kidney. Otherwise I’ll never get rid of it. The breathing sounds and cough is better too so maybe that is a result of the extra medication. Problem is that I still need to find a sleep aid if I can’t use Tylenol PM.

Also, even though it feels like the numbness is better, I still don’t feel great. The vascular surgeon wants me to ask the dialysis team to start using the fistula tomorrow. I think you have to sit very still in case the needle comes out, whereas the tubing is locked to the catheter. I don’t know if I’m ready for it with the current neuropathy levels and the need to move around in my chair.
Peripheral Neuropathy 3/10/2020 (updated)
Wow, the numbness and tingling in my feet is driving me crazy today. It felt really intense this morning while I was trying to sleep. The combination with my chest pains kept me from falling asleep all night/morning. Now during dialysis, it feels even worse and I’m not sure why. My weight and fluids are not that high compared to last session.
I don’t know what to do. There’s still 2.5 hours left and I’m starting to feel like I did that time in December when I had to go to the ER. I don’t want that again.
==========
I asked the technician if I can stand up and stretch my legs and he said no. I think they’re really worried about low blood pressure and me fainting if I stand up. My sitting blood pressure is at 152/85 so I think it’s ok to stand. Anyway, he gave me a paper towel soaked in ice water to put on my head and neck. That helped to cool me down a bit but doesn’t do anything about my neuropathy. I feel a bit better and sitting up as much as possible to stretch my left leg but it still sucks. 2:04 left on the dialysis timer…
==========
There’s an old Hispanic guy in the chair in front of me. He’s confined to a wheelchair and I’ve never heard him speak English. He alternates between sleeping and looking over at me. I’m not sure what he wants.

==========
19 minutes left. I’m not sure how I lasted this long. My nephrologist came by on her rounds so that distracted me for 15 minutes. The problem is they lowered my dry weight some more to 90 kg.
16 minutes left. I was going to ask them to let me off a few minutes early since my session will end right at 1:00 pm and I have another appointment at 1:15 pm right across the street. It’s really busy in here though. I’ll try to put on the manual tie-on mask now to save time.
==========
It’s now 6:20 pm and at home. I had an appointment to see the vascular surgeon after dialysis. The plan was to go to cardiac rehab after that but I was so tired that I just came home around 2:00 pm. I then took a long nap since I did’t sleep this morning but when I woke up, the numbness and tingling in my feet was even worse, if that’s possible. I had to walk around the upstairs hallway in my house to try and get the feeling to subside.
Chaplain Intern, Part II
The Korean chaplain intern stopped by again today. So far, he just dropped off a piece of paper. It looks like he’s starting a weekly newsletter and coming by the dialysis clinic on Thursdays and Fridays. On the newsletter, called The Rainbow Weekly, he translated a Korean poem titled 꽃 (The Flower) by Kim Chun-soo. There’s a different translation here.
I’m not sure where he went after dropping off the poem. He said he’s here from 8:00 am to 5:00 pm so maybe I’ll get to talk to him before I’m done today. I wonder if he listens to K-pop.
Dialysis 2/29/2020
Arg! The numbness in my left foot is driving me crazy today. It was not that bad this morning but started getting worse as soon as I sat down in the dialysis chair. I’ve been watching YouTube videos and thought a lot of time has passed but in reality, it was only about an hour. There is still 2:35 left on the dialysis machine. Where is my fast forward button?!
I’m in a new seat today. Not sure how the musical chairs work but I’m in the “other” corner of B pod. I hate sitting in the corners. You feel even more. Isolated from everyone and everything.

I also was able to take a clear look at another patient’s fistula. It’s in his forearm, purple, and about 1 x 2 inches in size. I hope my doesn’t end up looking like that or worse. It’s super ugly and gross.
URR Retest Results 2/20/2020
Finally, some good news. The previous clearance test came back as inadequate with an URR of 62.2%. I was afraid that they were going to extend my dialysis time again. However, since the dialysis machine alarmed several times that day, my nephrologist asked the clinic to run the clearance test again. Well, the results came back and the updated URR is 65.5%, which should be enough to clear me for another month. I really didn’t want to sit here longer then absolutely necessary.
Fistula Facts
One of the dialysis techs came by to check out my fistula. He said it looked and felt fine, then offered up some random information about fistulas.
- He said not to rush into using the fistula before it matures since it may blow out. If that happens, then I have to go back to the chest catheter. I didn’t ask him what happens if we’ve already removed the catheter. Also, I thought they (dialysis clinic + nephrologist) decided when the fistula is ready for use, not me.
- Even if the fistula matures, it could still blow out when used properly. I would rather keep using the chest catheter but everyone said I need the fistula.
- When the fistula is ready, they will start with only one needle in the fistula and connecting one of the ports on the catheter. I think this will continue to strengthen the fistula so it doesn’t blow out and fail. Not sure how long they will run with this “hybrid” connection. I guess the catheter is not going to be removed immediately.
- I need to exercise the fistula with a squeeze toy. The clinic gave me one that looks like a large pill to exercise and grow the fistula.

Dialysis 2/25/2020
Ugh, I feel terrible today. The neuropathy in my feet is probably the worst it’s even been. It feels like that time in December when I was sent to the ER from the dialysis clinic. It’s also hot in here for some reason. Usually it’s freezing inside the clinic but today, I had to get help to remove my jacket and it still feels warm. I can feel a panic attack coming and there’s over three hours left.
I also got only three hours of sleep this morning so I’m super tired. I’m called into my boss’s staff meeting right now and it’s hard to concentrate. I was going to cardiac rehab right after dialysis but I think I need to go home and take a nap. I still have two more appointments (therapist and acupuncture) this afternoon.
I’m actually a bit worried about my neuropathy and acupuncture. The numbness is probably not related to my Amiodarone prescription so likely acupuncture is having an effect. I do feel more in my feet but the numbness is increasing in intensity and feels worse overall than before.
==========
I came in to dialysis today at 94.5 kg. That’s 3.5 kg over my “dry” weight. My regular nurse is out sick so the substitute nurse asked me how much fluid to take out. We settled on 3.0 kg for today. I think there may be some correlation between lower leg edema and neuropathy intensity. It’s hard to control fluid intake on workdays with all the available free drinks. I usually start falling asleep late afternoons so need a cup or two of coffee to stay awake. If I was at home, I would just go and take a nap and skip the extra fluids.
Inadequate Adequacy Again
The dialysis nutritionist came by to tell me my labs were good, but the Kt/V numbest was inadequate. It was 1.16 this time; the minimum value is 1.20. Last time they increased my dialysis time by 15 minutes. They are going to redo the test but I’m probably looking at four hour sessions until my fistula matures. Like I said before, just when you think you life can’t get any worse, another negative surprise is just around the corner.

Dialysis Blood Pressure 2/6/2020
I’m still writing down blood pressure readings during dialysis, trying to figure out the pattern and how to minimize the fluctuation. Here are some readings from today:
| Time | Systolic | Diastolic | Pulse | Notes |
| 8:50 am | 127 | 73 | 65 | Standing |
| 8:55 am | 137 | 78 | 63 | Sitting/legs up |
| 9:07 am | 148 | 83 | 63 | Sitting/legs up |
| 9:38 am | 131 | 77 | 63 | Sitting/legs up |
| 11:08 am | 178 | 88 | 65 | Sitting/legs up |
| 11:38 am | 156 | 88 | 65 | Sitting/legs down |
| 12:45 pm | 171 | Sitting/legs down | ||
| 1:00 pm | 131 | Standing |
I can’t remember what I was doing between 9:30 am and 11:00 am but I missed several readings. My nephrologist agrees that likely the Metoprolol is being dialyzed out of my bloodstream during dialysis but she doesn’t want to prescribe more drugs yet. She did say the both the Metoprolol (beta blocker) and Olmesartan (ARB) are good for heart disease patients. NIFEdipine, even though it works great on me, doesn’t have any heart protection properties.
I handed a copy of my Medicare card to the front counter person. She said she will give it to my dialysis social worker. I hope they know how to coordinate billing since Medicare is supposed to pick up whatever my insurance does not pay. That is probably ~$3,000 since I am responsible for 85% of dialysis costs until I hit my out-of-pocket max. I still don’t know if Medicare covers my work insurance co-pays because I paid $280 already just for acupuncture co-pays.
What is Dialysis?
I use terms like hemodialysis and peritoneal dialysis often but most people probably don’t know what that means. I sure didn’t know anything about three years ago. I found some nice pictures online.
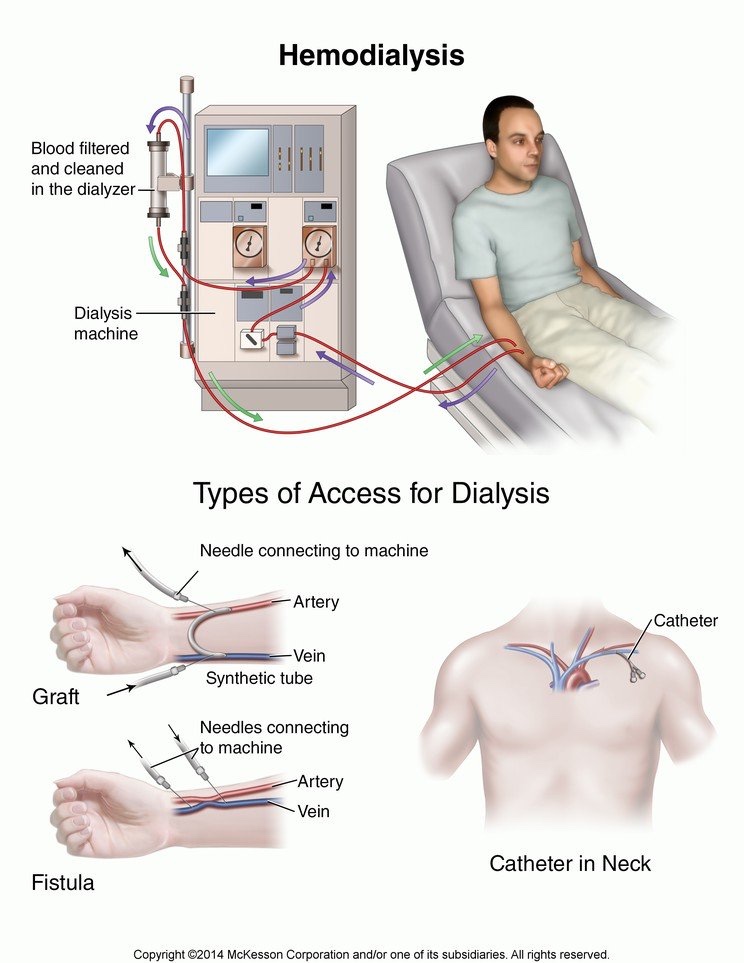
I go to the St. Joseph Hospital Renal Center three times a week for hemodialysis. It’s a non-profit dialysis center. Most patients are at a for-profit center like DaVita or Fresenius. Currently I have a catheter in my chest, my second one. I just had surgery to put in a fistula in my right arm above the wrist. When that matures and works, I’ll need to have the catheter removed, again.
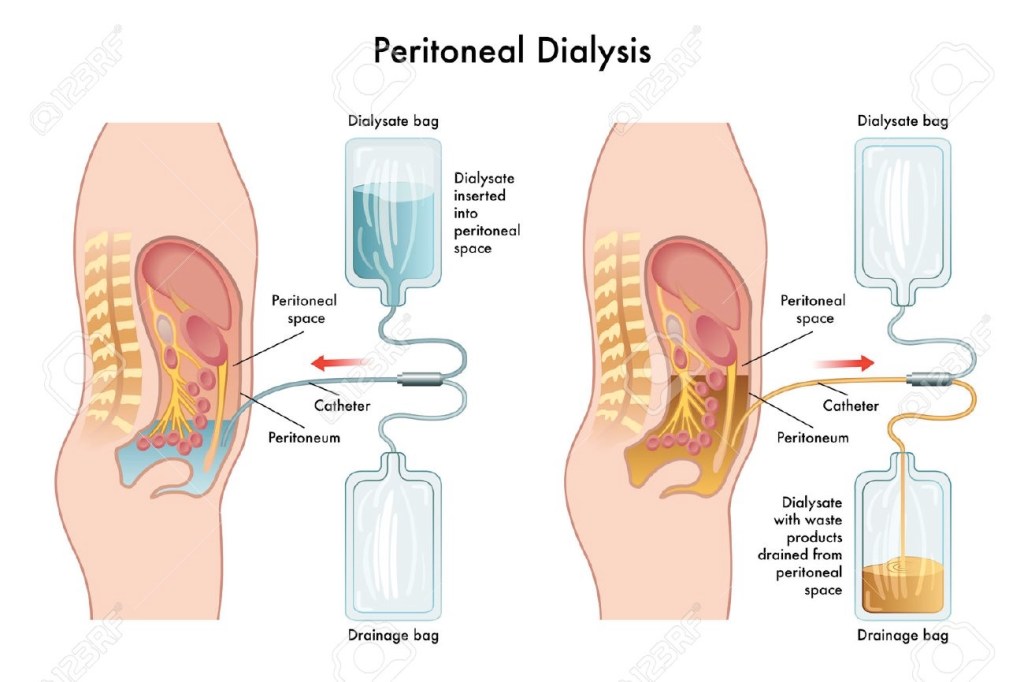
For six months I switched to peritoneal dialysis which required a different catheter. That was put in during April last year. Basically you put a dextrose solution in your abdominal cavity and let osmosis remove toxins and excess fluid by passing them through your abdominal wall membrane. The used solution is then drained and disposed. This fluid exchange can be done manually 4-6 times a day, taking about an hour each time.

For me, instead of using manual exchanges, I has a machine that basically pumps fluid in and out of my abdomen overnight so I can work during the day with minimal interruptions. I would attach three bags of dextrose solution totaling 15 liters and the machine would cycle the fluid five times in and out of my abdomen. I also had to do a manual exchange around noon each day for extra dialysis. It turned out that my peritoneal membrane wasn’t suited for dialysis so I had to stop and go back to hemodialysis during the same time as my heart bypass surgery.

Also available is home hemodialysis. Basically it’s a different machine that allows you to do dialysis at home. If my living donor kidney transplants don’t work out, that may be an option for me later.
Renovations
They finally renovated the lobby of my dialysis clinic. Their initial Medicare certification date appears to be 8/15/1977 so the center been around 40+ years, and the previous furniture in the lobby looks about that old. They also replaced the carpet with laminate wood flooring so it looks more clean and modern. For some reason, there are less chairs now so when the center is busy, there are not enough seats for all the patients waiting to be called.

They also covered the walls inside the clinic with huge murals of scenery from tropical islands. The mural on my side of the clinic is a sunset scene so everything is very orange. You can see a bit of it on the left in the photo below. The wall used to be just beige.

Fistula Show & Tell
I drove to dialysis today by myself even though I was supposed to wait 24 hours. I was going to ask my dad to drive me but by the time I remembered, I was already on the road.
I showed my dialysis nurse the bandage on my right arm and told them I had the surgery done. A couple of nurses came by to take a look and they were more excited about the surgery than I was. I think they really don’t like using the chest catheter unless it’s absolutely necessary. One of the supervising nurses pulled out her stethoscope, listened to the surgery site, and gave me a thumbs up. Not sure what she was listening for but I’m glad it was good.

They continue to challenge my weight at dialysis. Even though my dry or ideal weight is 92.0 kg, they try to take more fluid out since they want to avoid edema or having fluid build up in the lungs. I left dialysis at 90.9 kg; that’s probably my lowest ending weight in over two years of hemodialysis.
Dialysis Blood Pressure 1/30/2020 (updated)
I fell asleep early last night and woke up at around 3:30 am this morning. I thought I didn’t take my 30 mg of NIFEdipine ER before sleeping so I took another one. I then took all my regular medications this morning, including the 10 mg of NIFEdipine.
When I got to the dialysis clinic and measured my standing blood pressure, it was 90/60. Either I doubled up on the ER pill, or took it too late so it’s adding to the three medications I took this morning. That’s one issue with having too many meds. You lose track of which ones you took when sometimes.
The first blood pressure reading sitting down was 120/69 which is still a bit too low. It should increase when the Metoprolol starts getting dialyzed out by the machine.
==========
Ha! The machine too another blood pressure reading while I was clicking “post” on this post. It first came back as 78/50. I told the nurse that can’t be right so she tested again and it came back at 110/64. Better, but I definitely messed up my medication schedule this morning.
==========
| Time | Systolic | Diastolic | Pulse | Notes |
| 8:45 am | 90 | 60 | — | Standing |
| 8:46 am | 102 | — | — | Standing |
| 8:53 am | 120 | 69 | 59 | Sitting/legs up |
| 9:23 am | 110 | 64 | 63 | Sitting/legs up |
| 9:58 am | 134 | 71 | 59 | Sitting/legs up |
| 10:28 am | 139 | 82 | 59 | Sitting/legs down |
| 10:58 am | 139 | 82 | 60 | Sitting/legs down |
| 11:28 am | 145 | 87 | 59 | Sitting/legs down |
| 11:58 am | 158 | 95 | 60 | Sitting/legs down |
| 12:28 pm | 163 | 93 | 58 | Sitting/legs up |
| 12:58 pm | 178 | — | — | Sitting/legs up |
| 1:03 pm | 138 | — | — | Standing |
So the systolic numbers goes really high right at the end. I’m thinking the 178 reading is wrong since it then drops by 40 points on the last standing measurement. With such huge variations in blood pressure readings over four hours, it’s all dependent on the level of medications in my bloodstream. I feel like I’m cheating each time I take the extra 10 mg of NIFEdipine since it’s like an emergency drug: works quickly and wears off fast. I measured my blood pressure yesterday around 2:00 pm and it was 192/100. All the morning meds probably wore off by then. I don’t think it’s good for my body to have blood pressure fluctuate like that.
I check the dialysis blood pressure measurements from the past few sessions and the drop in blood pressure for the last standing measurement is pretty large. That just makes prescribing medication that much harder since they can’t lower my sitting blood pressure too much in case I stand up and pass out.
| Date | Last Sitting BP | Final Standing BP |
| Jan 21 | 165/98 | 139/82 |
| Jan 23 | 164/90 | 132/78 |
| Jan 25 | 159/92 | 127/74 |
| Jan 28 | 163/87 | 118/70 |
| Jan 30 | 178/– | 138/– |
Can you say orthostatic hypotension?
Nurse Rotation
There are four “pods” at my dialysis clinic and each is staffed by a nurse and one or two technicians. I used to be in C pod previously but now I’m in B pod after switching shifts. They rotate the staff around so if you stay here long enough, everybody gets to work on you. I think the technicians rotate every three months and nurses rotate every six months.
Today is the first nurse rotation since I came back to this dialysis clinic. In total, there are four regular nurses and two supervisors that fill in when it’s busy, or if someone is out. Most are Filipino with one Hispanic and one Korean nurse. I know all of them pretty well because only the nurses can connect me to the machine because I have a chest catheter instead of a fistula.
One of the nurses said that six months is too short since you get to know your patients better over time. I have to explain to the “new” nurse my blood pressure history and why I’m on three medications since it’s all new to her.
Dialysis Facility Compare
I’ve been so focused on researching transplant centers that I didn’t realize Medicare rates dialysis facilities. I searched for my dialysis clinic, St. Joseph Hospital Renal Center, and they only have a 4/5 star rating for quality of patient care, but a 5/5 for patient survey. Looking at the rating details, I think they got dinged for a lower % of adult patients who had enough waste removed from their blood during hemodialysis. That explains why they want me to increase my dialysis time when my Kt/V result came back at 1.18 (should be at least 1.2). Across the street from my dialysis clinic is Satellite Healthcare Orange, which was my center for peritoneal dialysis. They have 5/5 stars for both ratings; maybe I should have gone there for hemodialysis instead of returning to St. Joseph. There is also a DaVita facility nearby. They have a 5/5 from Medicare but only 3/5 from their patients.
Some other interesting statistics:
| DaVita | St. Joseph | Satellite | California | National | |
| Preventing bloodstream infections | As Expected | As Expected | Better than Expected | ||
| Adult patients who had enough waste removed from their blood during hemodialysis | 96% | 89% | 97% | 96% | 97% |
| Adult patients who had enough waste removed from their blood during peritoneal dialysis | 97% | N/A | 93% | 89% | 91% |
| Rate of fistula | Better than Expected | As Expected | As Expected | ||
| Adult patients who had a catheter (tube) left in a vein for at least 3 consecutive complete months for their regular hemodialysis treatments | 8% | 12% | 6% | 13% | 13% |
| Frequency of hospital admission | As Expected | As Expected | Better than Expected | ||
| Frequency of hospital readmission | As Expected | As Expected | As Expected | ||
| Rate of patient death | As Expected | As Expected | As Expected |
As I was debating the fistula surgery, I noticed most of the patients at St. Joseph is getting dialysis through a fistula. From the data above, there’s more catheters at St. Joseph than at DaVita and Satellite. Medicare states that higher rate of fistula is better, and lower usage of catheter is also better. This also likely affected St. Joseph’s Medicare rating. Sorry!
For patient survey, DaVita got average ratings for kidney doctors and clinic staff, while St. Joseph and Satellite got better than average numbers.
More Dialysys Time
Crap! Just what I need in my life right now… more time on the dialysis machine. My nephrologist came by today during dialysis and told me my last Kt/V result was 1.18 even though my URR was 65%. Minimum clearance for hemodialysis is 1.2. She was fine with the number but the dialysis clinic is unhappy. I think they are regulated very closely by the state department of health, and it looks bad if a patient is not getting adequate dialysis.
Since I’m still using a chest catheter, the maximum flow rate is 350 mL/min and I’m maxed out. A mature fistula can work at 600+ mL/min so more blood flows through the machine and filter. Starting next session, we’re adding 15 minutes each day to my dialysis time. It sucks but I guess it’s better than adding 30 minutes.
Incidentally, about 7% of body weight is blood so at 92.0 kg, I have about 6.5 liters of blood. At 350 mL/min for 3.5 hours, that means the machine can filter 73.5 liters of blood or 11.4 times my blood volume. That filter is not very good. In comparison, for a 70 kg male adult, blood flow through the kidneys is 1.2 – 1.3 liters per minute
Dialysis Blood Pressure 1/25/2020 (updated)
The medications continue to work. I took all three at around 8:15 am this morning before dialysis. Here are the first several readings:
| Time | Systolic | Diastolic | Pulse | Notes |
| 9:02 am | 117 | 74 | 64 | Standing |
| 9:13 am | 135 | 75 | 63 | Sitting/legs up |
| 9:43 am | 141 | 79 | 60 | Sitting/legs up |
| 10:13 am | 151 | 83 | 60 | Sitting/legs up |
| 10:43 am | 145 | 86 | 60 | Sitting/legs down |
I only have two data points since I started taking all three medications before dialysis, but if you look at the numbers from last session, my blood pressure increased at the 10:18 am reading. Likewise, there seems to be an increase today at 10:13 am. One or more medication is getting dialyzed out about an hour into dialysis. My guess is the Metoprolol. There was a study done on Olmesartan and it appears resistant to dialysis.
==========
Blood pressure increased to 168/96 at 11:43 am. Either something else is getting dialyzed out or the 10 mg of NIFEdipine is wearing off since it’s such a low dose.
==========
Remaining readings continued from table above:
| Time | Systolic | Diastolic | Pulse | Notes |
| 11:13 am | 148 | 90 | 60 | Sitting/legs down |
| 11:43 am | 168 | 96 | 62 | Sitting/legs down |
| 12:13 pm | 156 | 88 | 60 | Lying down |
| 12:43 pm | 157 | 89 | 62 | Lying down |
| 12:50 pm | 159 | 92 | 62 | Sitting/legs down |
| 12:52 pm | 127 | 74 | 65 | Standing |
I’m surprised that both number dropped so much on the final standing measurement. The initial increase at the beginning of dialysis when I sat down wasn’t that large. That means I still have orthostatic hypotension.