I am not sure what the right title should be for this post, but I ran into several issues today, and they are likely related to the overly complex medical delivery and insurance system we have here in the United States.
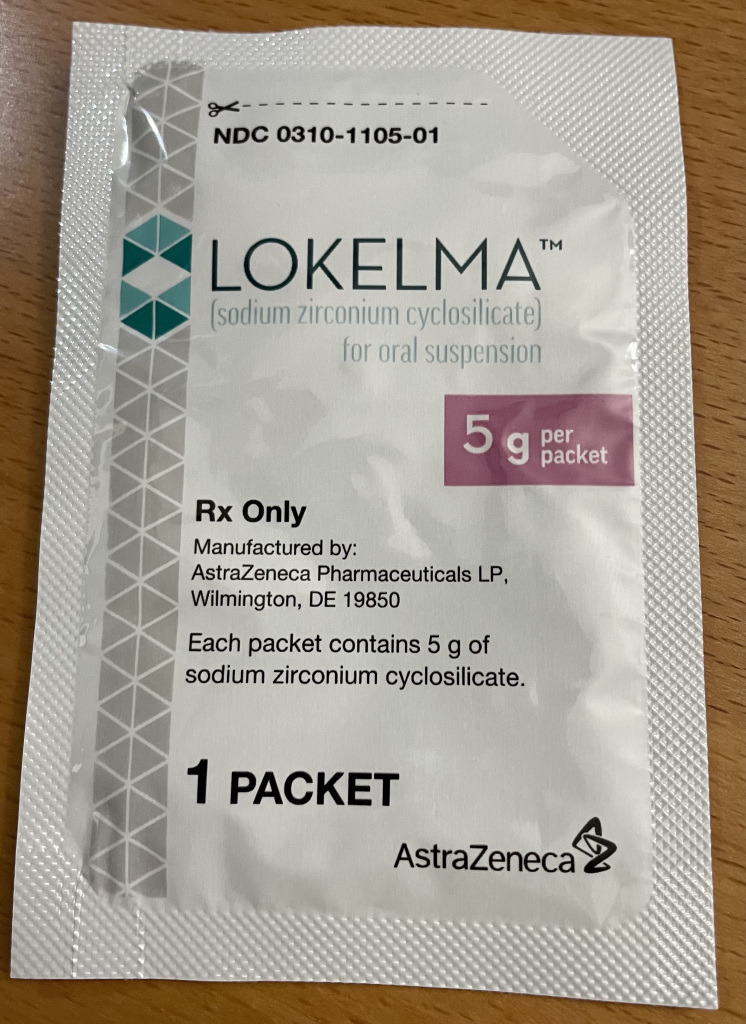
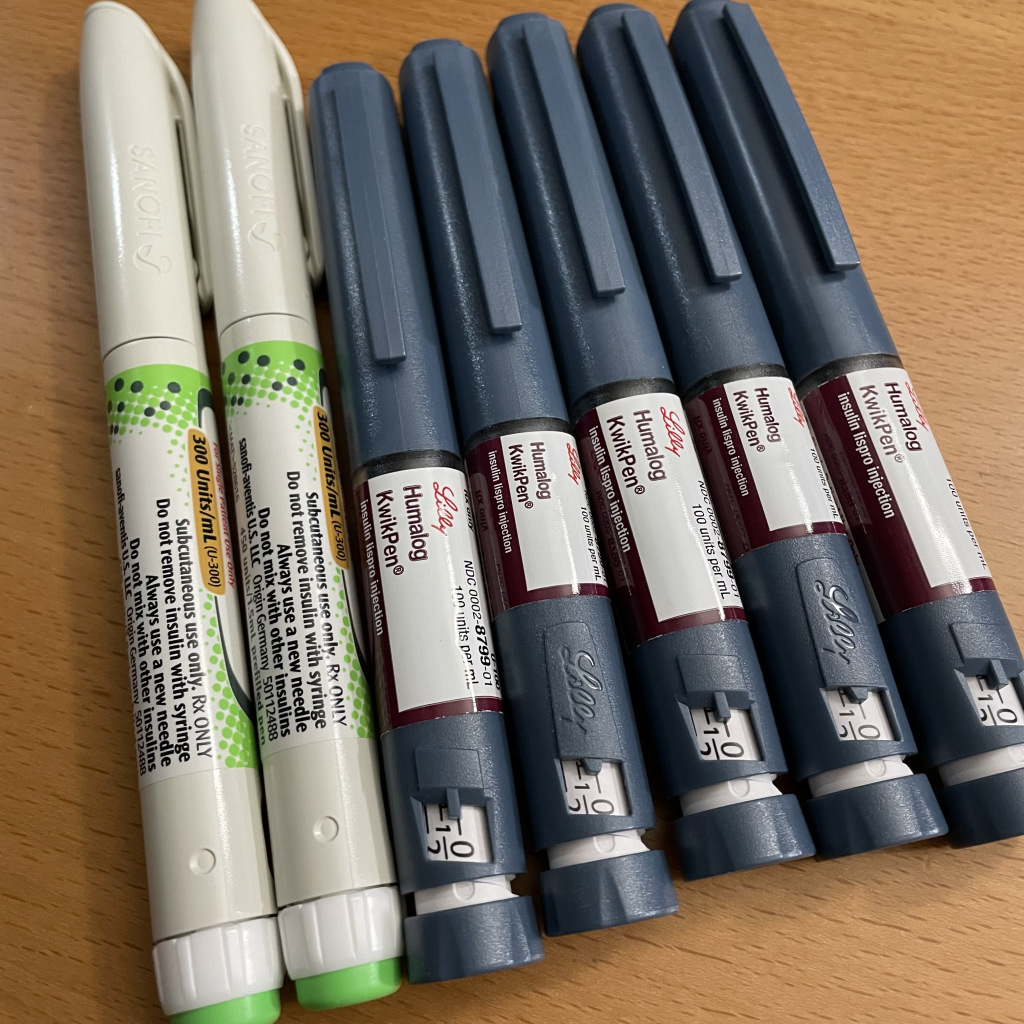
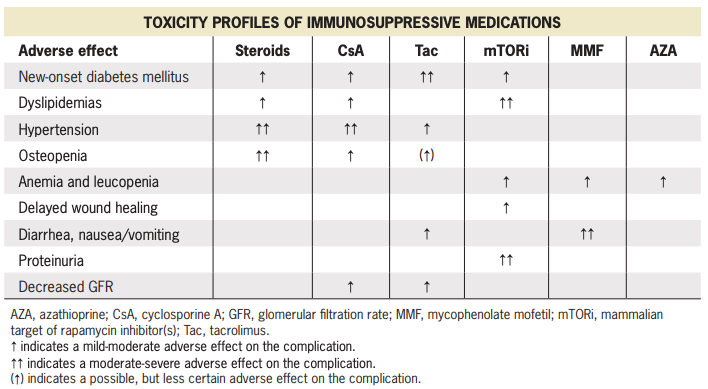
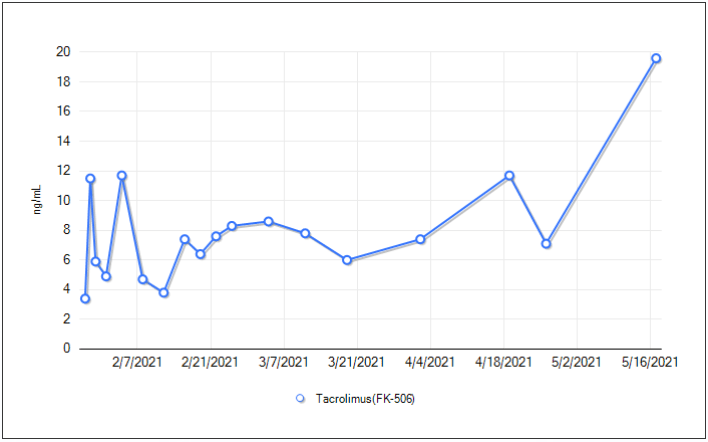
Since my nephrologist increased my dosage of tacrolimus, I needed a new prescription so I do not run out. I had them send it to my regular pharmacy which does not accept Medicare Part B, but have filled a previous prescription for tacrolimus for $10. This time however, the pharmacy said my work insurance would only pay a portion, and my co-pay would be ~$140. She looked into they system and could not figure out why it was only $10 last time, but a lot more today. I told them to hold on to the meds until I called my insurance.
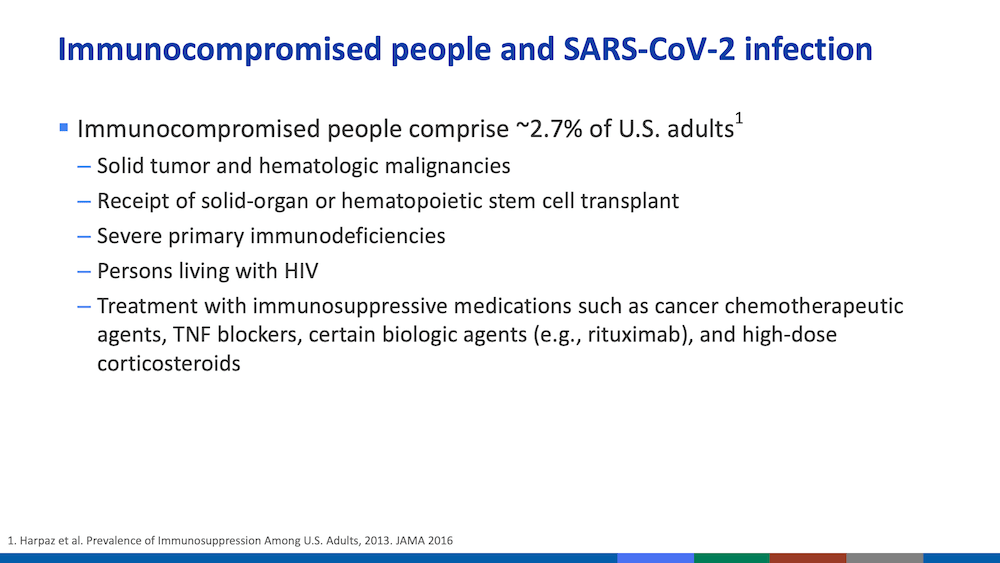
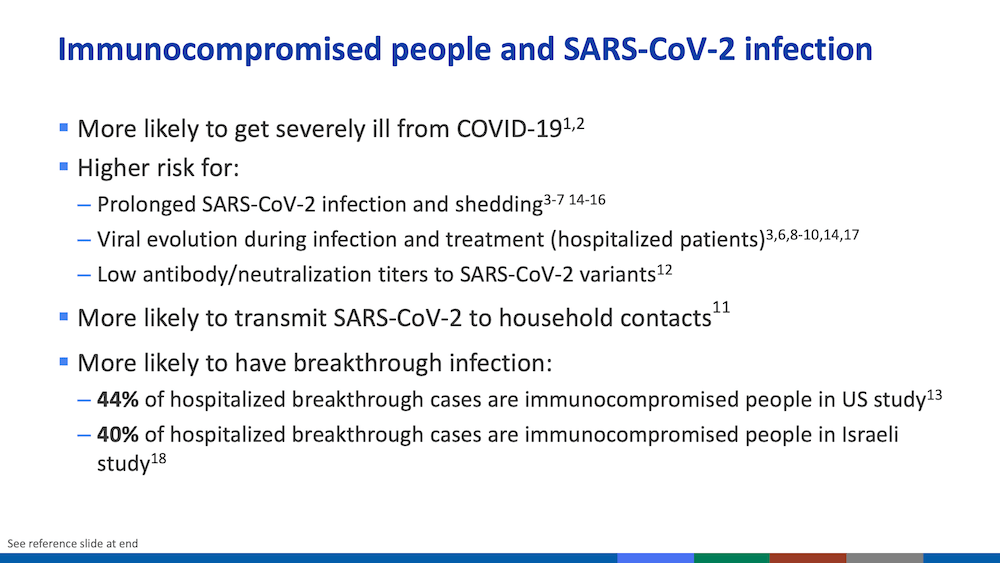
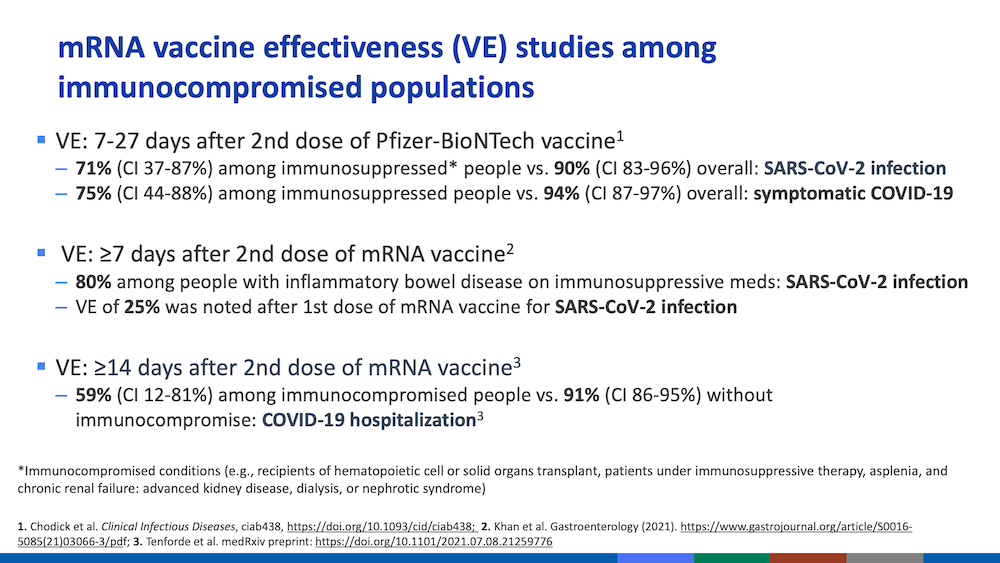
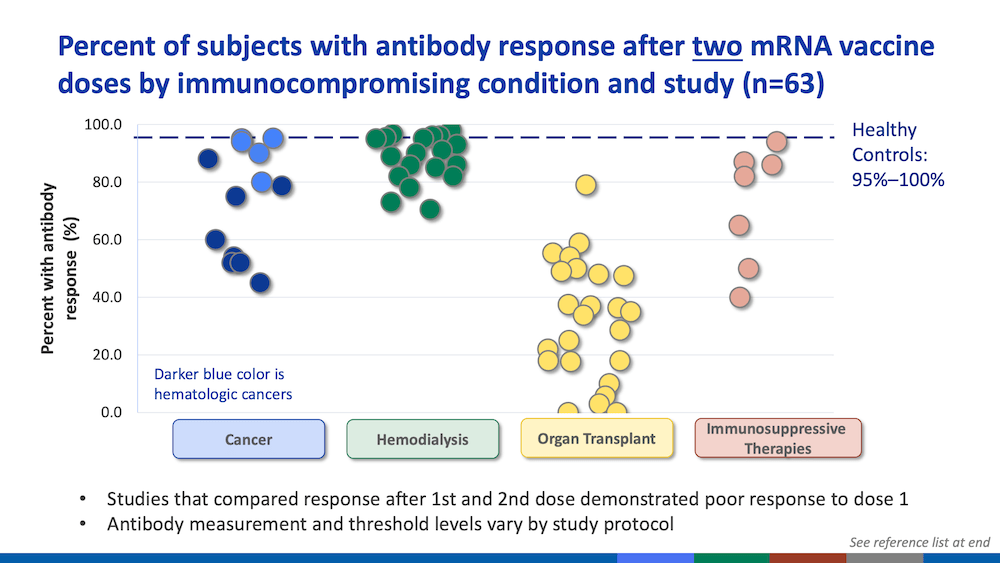
While I was at the pharmacy, I asked them about a second vaccination. They said they were not allowed to offer another shot to anyone that is already vaccinated due to FDA rules. Now that all our vaccination data is in a database, it is easy to check everyone’s vaccination status. The pharmacist basically said the only way is to lie about your vaccination status but I do not know what happens whey they try to enter my data (again) into the vaccination database. I was told to wait for the FDA to make a determination but that will takes months since there does not seem to be any urgency for the 2.7% or ~10 million Americans that are immunocompromised.
==========
I just called my work insurance and no one was available to answer the call, so I left a voicemail. I also called UCLA pharmacy about accepting prescriptions from outside the UCLA Health system, and they said it was no problem. I guess I have to cancel my order at my local pharmacy and have my nephrologist resend the prescription script to UCLA pharmacy.
==========
Sigh. Just as I clicked Publish for this post, a “get vaccinated” commercial came up on the TV set.